I know that “self-care” is this phrase that gets thrown around a lot, but there’s a reason for that. It’s critical to take care of yourself so that you can be your best self for others.
When you’re a mom, there are people depending on you and it’s important that you are able to be there for them.
That starts with taking care of you.
I know that it’s easier said than done.
Trust me. I know how busy you are. I am a mom too. When my seven kids were younger, I hardly had a moment to myself.
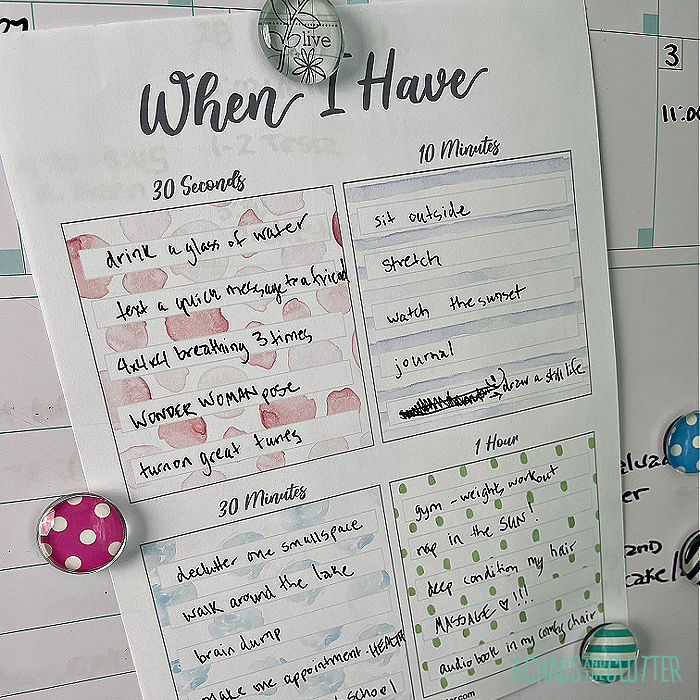
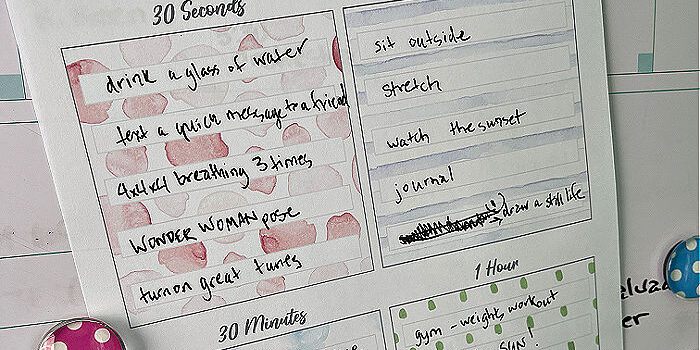
And that’s why I designed this self-care plan to have realistic time frames for those self-care opportunities you get in a day.
You may not be able to take an entire afternoon for yourself. Most days, you won’t be able to even take half an hour, but 30 seconds or ten minutes? That you can do!
So these ideas are designed for you to be able to take those little pockets of time and use them in ways that will most benefit you.
How to Create your Self-Care Plan:
- Download your free copy of the Self-Care Plan.
- Sit somewhere quiet that’s comfortable for you and go through the ideas listed on the pages inside.
- If you’re in that season of life when you don’t have anywhere quiet, lock yourself in the bathroom for a few minutes.
- Think about each activity and how you feel after you complete something like it. Circle the ones that resonate with you as making you feel rested, renewed, recharged, energized, or peaceful.
- Take the time to consider what works best for you. Just because going for a run makes your friend feel great, doesn’t mean you have to feel the same way!
- Put the lists away for a bit.
- The next time you have a few minutes to yourself (preferably within a day or two), come back to the lists and choose the circled activities that most jump out at you.
- You may write those in the corresponding section in your self-care plan or open in Adobe PDF and type in your list. Once you type it in, you can save it and print!
- Hang your plan somewhere you will see it often such as on your fridge, next to your calendar, or in a room where you spend a lot of time.
A few things to note for this self-care plan:
Feel free to move things from one list to another. The timelines are just a guideline. There are some activities that could belong on several of the lists so feel free to place them where you feel they would work best for you.
Be as specific as you can be for your personal chart. Where in the suggestions, you might see “learn”, for you that might be “research ancient Roman historical fashion” or it may be “practise Spanish”. The more specific you are, the more likely you are to follow through.
Some of the activities are ones that aren’t necessary to do again and again so if you complete some of those, you can print yourself off another chart and fill it in with new activities. While you’re at it, congratulate yourself for how well you are doing on your self-care journey!
A special thank you to my lovely friend, Heather for allowing me to bring this concept to you!
There are suggestions included to help get your creative juices flowing for each allotted amount of time.
When you have 30 seconds:
- Take 3 deep breaths.
- Splash cold water on your face.
- Drink a glass of water.
- Give yourself a high five in the mirror.
- Speak 5 things you’re grateful for.
- Forgive yourself.
- Compliment a stranger.
- Smell a flower.

- Light a candle.
- Cuddle a pet.
- Hug a human.
- Turn on music.
- Text someone an encouraging note.
- Smile!
- Give yourself credit.
- Do the Wonder Woman power pose.
- Set a boundary.
- Speak an affirmation.
- Squish playdough.
- Give up trying to be perfect.
- Squeeze a stress ball.
When you have 10 minutes:
- Enjoy a cup of tea.
- Enjoy a cup of coffee.
- Wear something you love.
- Set daily goals.
- Listen to great music.
- Call a friend.
- Sit outside.
- Pray.
- Eat something you love.
- Meditate.
- 10 minute tidy.
- Watch the sunrise.
- Grab a healthy snack.
- Stretch.
- Sing (loudly) in the shower or car.
- Paint your nails.
- Cuddle up under a blanket.
- Watch a funny video.
- Put up Post-it notes with inspirational quotes or scriptures.
- Sit in silence.

When you have 30 minutes:
- Go for a walk.
- Have a nap.
- Shower.
- Dance in your kitchen.
- Declutter.
- Journal.
- Read in the sun.
- Do yoga.
- Draw.
- Color.
- Listen to a podcast.

- Plan.
- Spread kindness to someone else.
- Have a picnic outside or in your living room.
- Do a brain dump.
- Puzzle.
- Play a board game.
- Plant something.
- Make yourself a doctor, dentist, or therapy appointment.
- Do something creative.

When you have one hour:
- Go for a walk.
- Have a nap.
- Shower.
- Dance in your kitchen.
- Declutter.
- Journal.
- Read in the sun.
- Do yoga.
- Draw.
- Color.
- Listen to a podcast.
- Plan.
- Spread kindness to someone else.
- Have a picnic outside or in your living room.
- Do a brain dump.
- Puzzle.
- Play a board game.
- Plant something.
- Make yourself a doctor, dentist, or therapy appointment.
- Do something creative.
There is that saying that failing to plan is planning to fail. By having a self-care plan ready, you can increase the chances of succeeding at finally putting yourself on the priority list.
If you are a foster or adoptive family, you may be interested in reading my book Self-Care for Foster and Adoptive Families.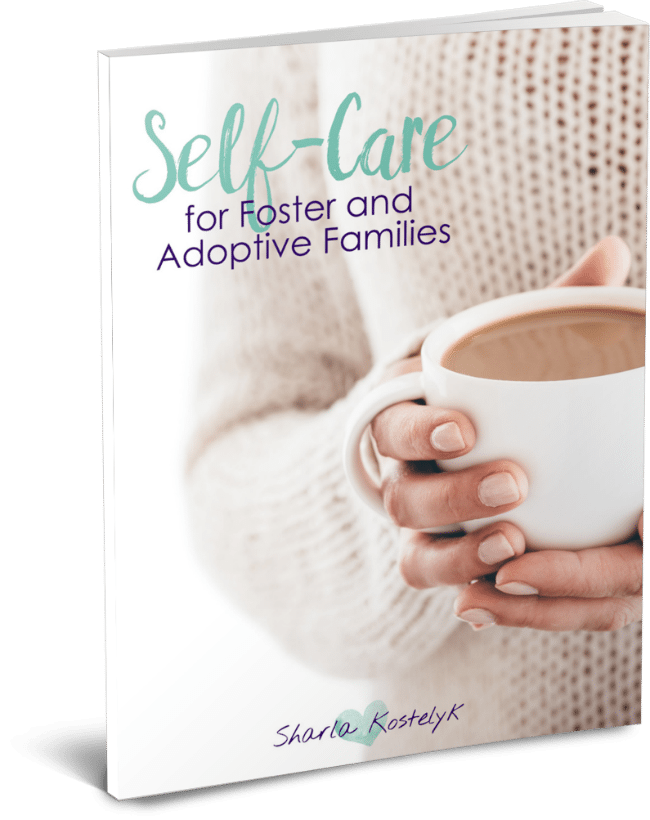

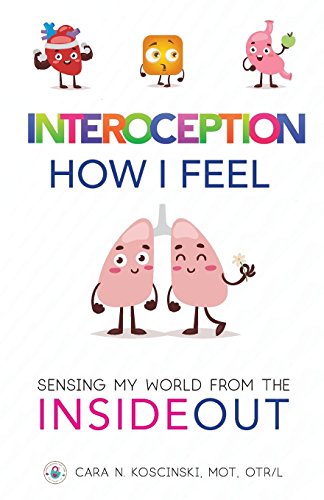
 So what is interoception? While the other sensory systems are focused on the perception of external sensations, interoception is the perception of internal sensations.
So what is interoception? While the other sensory systems are focused on the perception of external sensations, interoception is the perception of internal sensations. 










 Even if you don’t struggle with sensory issues yourself, I’m sure you can relate to the feeling of sensory overload. We’ve all been there. For some, it may be at a concert or crowded event. For others, it’s being in a gymnasium full of screeching preschoolers. Or perhaps for you, it’s
Even if you don’t struggle with sensory issues yourself, I’m sure you can relate to the feeling of sensory overload. We’ve all been there. For some, it may be at a concert or crowded event. For others, it’s being in a gymnasium full of screeching preschoolers. Or perhaps for you, it’s 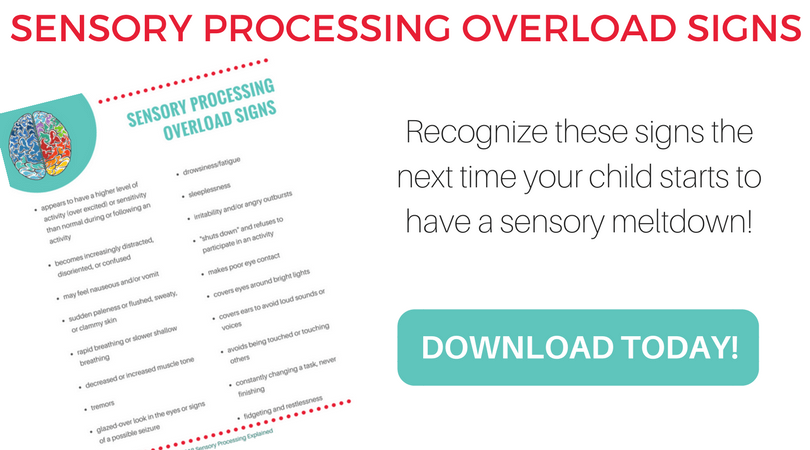



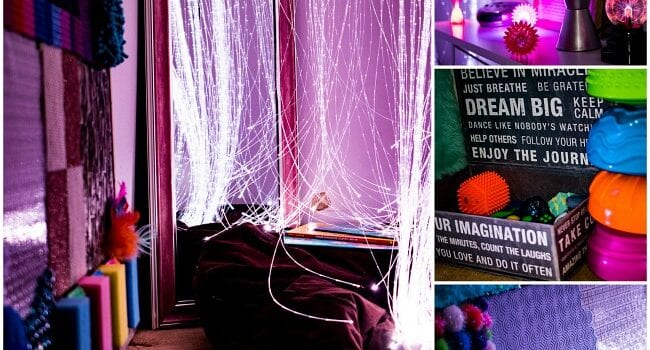
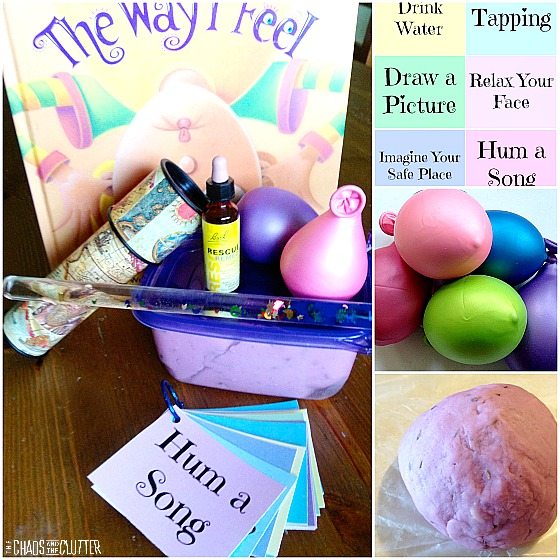
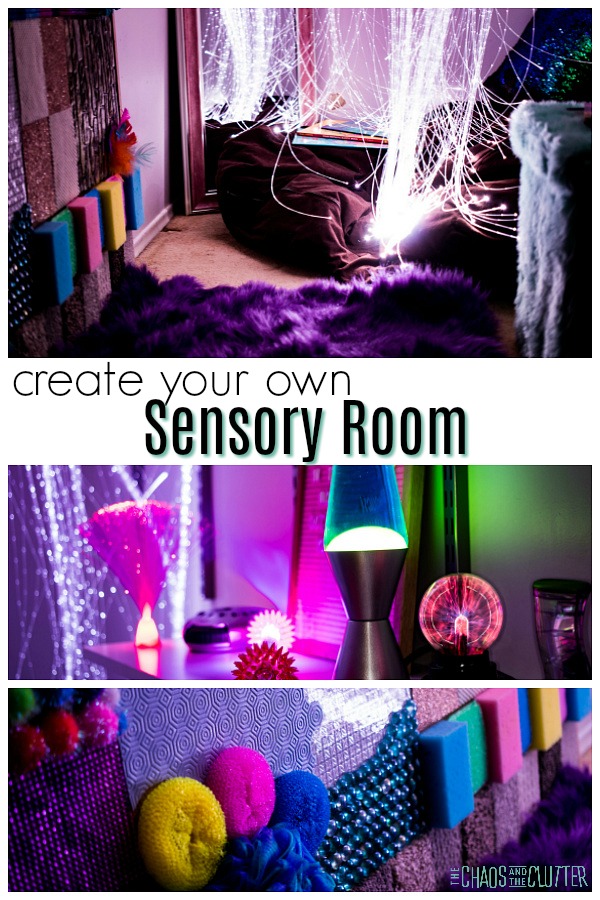 The kids got older. I still saw the need for a sensory room. I knew that if I didn’t create one now, they would soon be grown. That prompted my decision to use a storage closet as the space. I began planning how I could make things myself instead of purchasing expensive equipment.
The kids got older. I still saw the need for a sensory room. I knew that if I didn’t create one now, they would soon be grown. That prompted my decision to use a storage closet as the space. I began planning how I could make things myself instead of purchasing expensive equipment.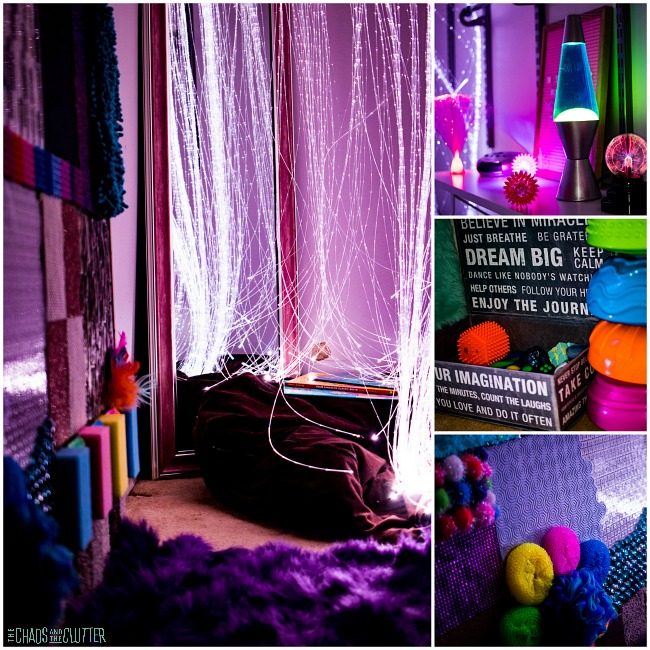 (photos courtesy of Shelley of
(photos courtesy of Shelley of 
 I placed a bean bag chair under the fibre optic light curtain and a mermaid pillow on top of the bean bag chair. I also have a few “brain friendly” books sitting there in case one of the kids wants to read while they are in the calm down corner.
I placed a bean bag chair under the fibre optic light curtain and a mermaid pillow on top of the bean bag chair. I also have a few “brain friendly” books sitting there in case one of the kids wants to read while they are in the calm down corner. 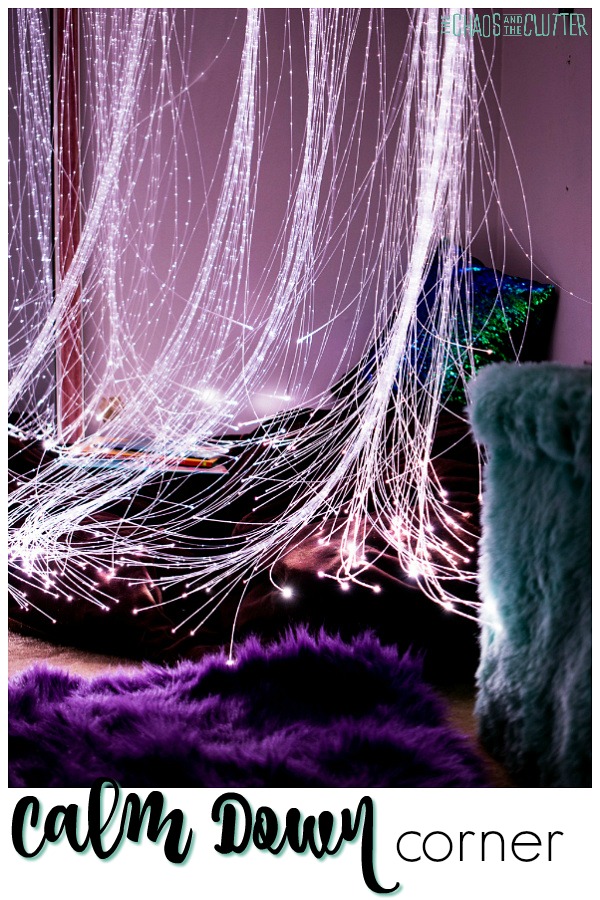 There is a long mirror across from that corner. This is for two reasons. The first is that the room used to be a storage closet so it’s very small and the mirror helps it feel bigger. The second is that kids can use the mirror to monitor their breathing and facial expressions which can help them to self-regulate.
There is a long mirror across from that corner. This is for two reasons. The first is that the room used to be a storage closet so it’s very small and the mirror helps it feel bigger. The second is that kids can use the mirror to monitor their breathing and facial expressions which can help them to self-regulate. The box contains all kinds of fidgets including pencil toppers,
The box contains all kinds of fidgets including pencil toppers, 










 On the felt board, I put the words “In Through Your Nose Out Through Your Mouth” as a reminder for my kids to do their
On the felt board, I put the words “In Through Your Nose Out Through Your Mouth” as a reminder for my kids to do their 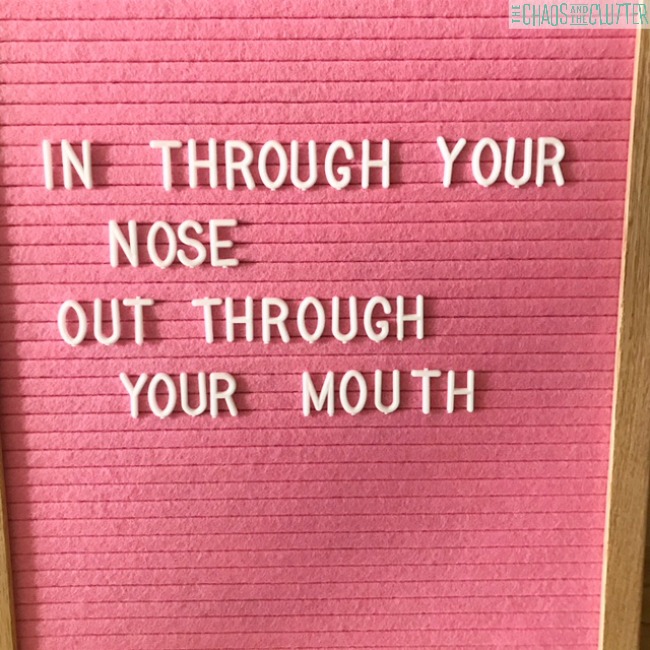













 The reason I share this list is to help parents and caregivers determine what stages are best for beginning to introduce
The reason I share this list is to help parents and caregivers determine what stages are best for beginning to introduce